

It’s hard to get anything done when your head is pounding. Add in common migraine symptoms like vision disturbances, nausea, and sensitivities to light or noise, and you’ve got a recipe for disaster.
Did you know that Thomas Jefferson suffered from severe headaches that many historians think were likely migraine episodes – he even dealt with one right before writing the Declaration of Independence!
His plight isn’t unusual. About 12% of Americans are affected by the intense pulsating headaches which can last anywhere from 4 hours to multiple days and can reoccur multiple times per week in some cases. Often passed down hereditarily, migraines are considered a disability when chronic.
WHAT’S A MIGRAINE – OR A HEADACHE FOR THAT MATTER?
Headaches are a common pain that most people deal with at one point or another, if not regularly. There are several types of headaches, and they aren’t dangerous, but they can be a symptom of a more dangerous condition. A migraine is a very severe form of a headache.
Migraine is a common, but severe neurological disease with a wide range of symptoms. There are several types of migraine episodes, but they all cause intense head pain, on one side or both, and often come with nausea, sensitivity to light, sound or smells. Women are three times more likely to experience a migraine episode than men.
Migraine episodes usually come suddenly, but sometimes sufferers get a warning through subtle changes like constipation, mood changes or food cravings. Then immediately before one comes on, an “aura” can foreshadow a migraine episode. Auras can present as bright flashing spots or lights in the sufferer’s vision, seeing wavy or jagged lines, speech changes and more.
HOW DO I IDENTIFY AND COMBAT MIGRAINE TRIGGERS?
Migraine episodes can be caused or intensified by a variety of different factors called “triggers,” and they can vary quite a bit from person to person. Common triggers include sensitivity to chemicals or preservatives in food, caffeine, daily use of pain-relieving medication, light, barometric pressure changes, not drinking enough water, overexertion and changes to regular sleep pattern.
One of the most common triggers by far is stress. During stressful situations, certain chemicals in the brain can cause a “fight or flight” response and then other emotional reactions like anxiety or worry actually make the problem worse by increasing muscle tension and dilating blood vessels.
>> WHAT TO KNOW ABOUT MENTAL HEALTH
After you learn your triggers, adjusting your lifestyle to eliminate them is a good start to attempting to curb your migraine episodes. If that strategy doesn’t stop the pain from coming, talk to a doctor about preventative medication. That way you can stop the headache before it shows up. You can also take medicines to combat the headache when it has already begun.
If none of that works, other methods can slow the pain. Rest in a quiet, dark room and switch between hot and cold compresses on your head. There are many forms of medication or therapy techniques doctors may advise for a migraine or chronic headache sufferer to try. Ask a doctor if you feel medication is right for treating your headaches.
HOW DO MIGRAINES AND HEADACHES AFFECT WORK?
Migraines send warning signals in the form of symptoms and auras. What if someone is at work when they realize a migraine is coming soon?
Try medicine. The first step to take is to find a quiet spot away from your work station, take preventative medication and relax. Wait for the headache to go away and return to work. If it doesn’t work, it might be time to consider going home.
Head home. Some people who regularly get migraines know a certain symptom will signify that it’s time to go home and try sleeping it off. If the medication didn’t solve the problem and symptoms are increasing or intensifying, it is probably time to go home before it gets any worse. If someone waits too long and the migraine is severe enough, it may be wiser to ask a family member, friend or coworker for a ride home or take public transportation, rather than driving impaired by the headache.
Sleep and get ready for a calm next day. If the migraine goes away after rest and sleep, then prepare to go to work but do not try to make up for the time missed. “When a patient misses a day because of a migraine or they’re behind because of a migraine, they get more anxious and concerned about finishing what they need to finish, and that doesn’t help the whole process,” said Dr. Merle Diamond, director of the Diamond Headache Clinic in Chicago.
>> WHY TAKING YOUR LUNCH BREAK MATTERS
Talk to your employer. If migraines are a regular problem you are dealing with, make sure your employer or HR representative knows your triggers and that there may be times when you need to go home. Advocate for yourself and make sure they know it won’t affect your work when unencumbered. Employers can support their migraine suffering employees by taking out bright lights or dimming the lights, asking the employee if they’d prefer to be moved to a more secluded or quiet area, make it clear you are flexible during an episode and by providing air-purification systems to reduce scents.
Want to be ready when a migraine episode begins? Make sure you have everything on your migraine checklist:
- Bottle of over-the-counter headache medicine and prescription medication if you have it
- Pair of sunglasses and ear plugs
- Bottle of water
- Tea bags or Instant coffee for the caffeine
- Cold and warm packs (keep the cold one in the freezer)
- Pair of headphones (if listening to music, audiobooks or podcasts soothes you)
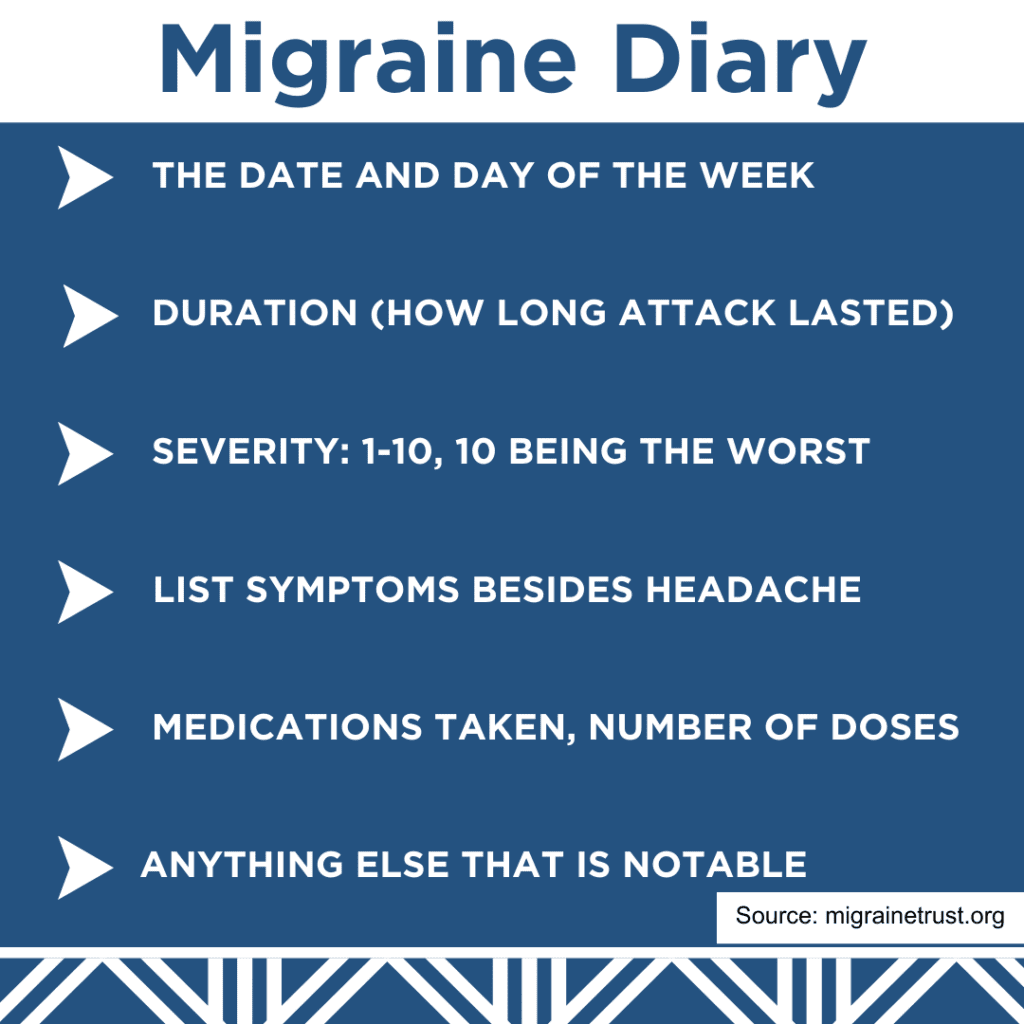
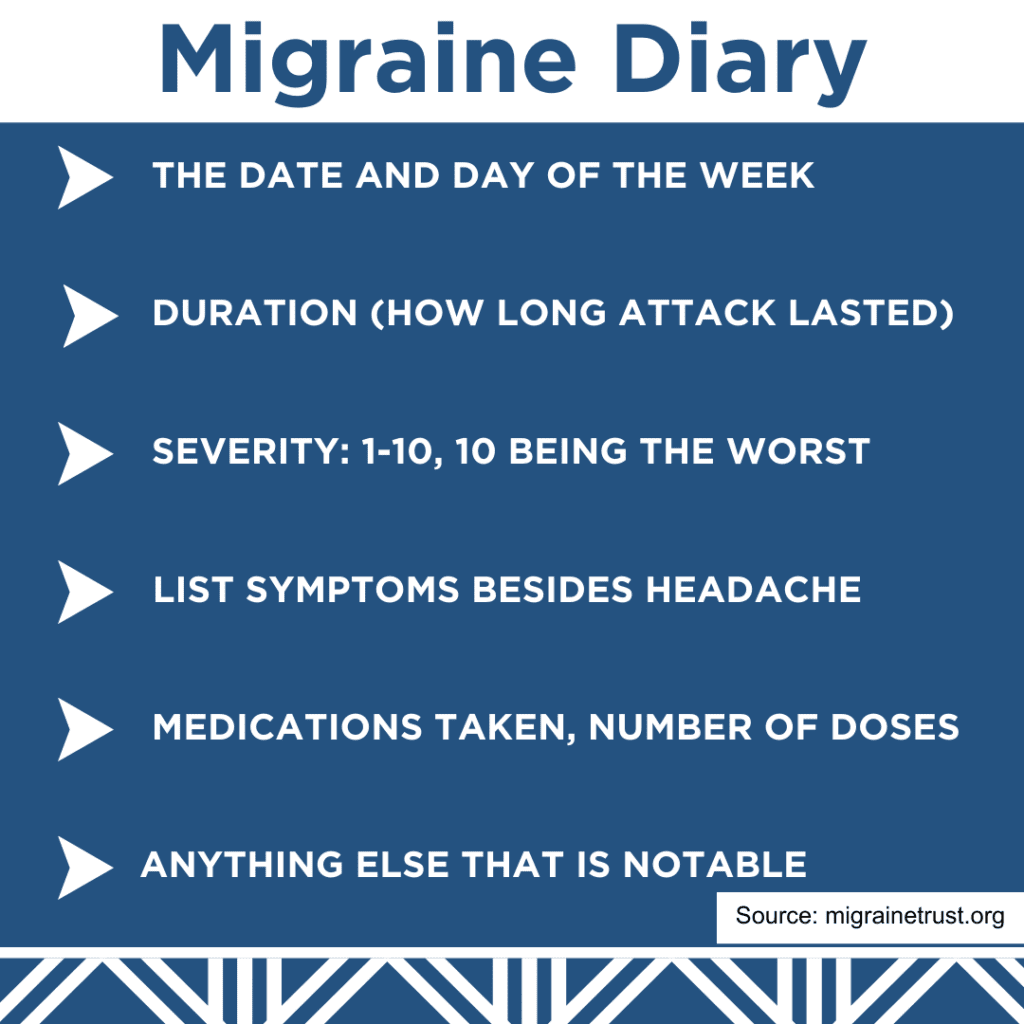
- Migraine diary
- Essential oils to dab on forehead or temples (lavender, peppermint, chamomile)
WHAT IF AN INJURY CAUSED MY MIGRAINES OR HEADACHES?
After suffering a traumatic brain injury, one of the most common symptoms is headache. Up to 90% of people with traumatic brain injuries report headaches and more than 30% of people report headaches that continue long after the injury occurs.
With about 1.4 million cases of traumatic brain injury occurring every year in America, headaches take on multiple forms after an injury. Stress headaches or cluster headaches as well as migraines and posttraumatic headaches can result from traumatic brain injuries. Keches Law Trial Attorney Sean Kiely said post-traumatic headaches act similarly to migraines.
“A migraine is considered a primary headache disorder. Whereas a Post-traumatic headache is a secondary disorder. They aren’t the same thing but they do have a lot of the common features,” Kiely says. “Things like light sensitivity, noise sensitivity, being nauseous, generally the symptoms that everyone associates with headaches are the same”
Kiely says nearly everyone who experiences a traumatic brain injury experiences a headache, but for some the effects are even worse.
“When somebody suffers a traumatic brain injury, oftentimes they will experience a headache in the immediate aftermath. It can range from up to 2/3 of those people will experience migraine-like symptoms up to a year after the injury,” he says. “With that being said, there are studies out there that suggest those who are susceptible to migraines prior to suffering a traumatic brain injury will experience an even worse effect of migraine-like symptoms after they suffer from a traumatic brain injury. It just exacerbates underlying problems.”
If a traumatic brain injury was caused by someone else’s negligence, recklessness or carelessness, then a personal injury lawsuit could be warranted.
ARE MIGRAINES COVERED BY WORKERS’ COMPENSATION?
Keches Law Senior Attorney Judith Gray says headaches, may be compensable as a symptom of a work injury.
“If a headache results in a disability from performing your job, or a modified job and it can be established that the symptoms are medically causally related to the injury sustained at work, the resulting disability may be compensable” she says. “For example, if a Court Officer is attacked by an inmate and suffers a head injury, with symptoms to include debilitating headache which prevent him/her from performing their job duties, this injury would likely be compensable under M.G.L. c. 152.”
However, Gray points out that the cause of the headaches must be work-related.
“If an individual suffers from migraine type headaches unrelated to any workplace injury and/or has actively treated for headaches unprecipitated by a work injury for years, the simple act of suffering a migraine at work generally would not be compensable,” she says.
In fact, Gray says workers’ compensation for headaches is a medical decision and will require a physician to relate the headaches to an event or series of events that happened at work. She says in some cases the physician also needs to distinguish the workplace headaches from a prior condition or treatment the employee had undergone.
All sick-leave and paid time off need to be used before disability is claimed. The other issue is that the person’s migraines need to qualify as a disability.
A disability is usually described as a condition, injury or illness that renders a person unable to do his or her job. If someone wanted to claim workers’ compensation for migraines, they would need to provide proof to the insurance company through documentation of their migraines.
>> ELIGIBLE FOR A WORKERS’ COMP STRESS CLAIM?
Keeping a “migraine-diary” stating how long each migraine lasts and what symptoms develop is a good way to present evidence as proof, not to mention a good way to gather information for a doctor.
TURN TO KECHES LAW GROUP FOR HELP
Headaches and migraines are a harsh everyday reality for millions of people in America. If you are considering filing for workers’ compensation or a personal injury lawsuit, know that we are here to help and can guide you through the process.




